MocDoc's Offerings
What are the different types of healthcare software?
Published By
Steve
2019051816:52:15
Category Healthcare

The healthcare sector is facing pressure to move to digital systems, both from regulatory authorities and from the general public. The government is pushing for digital systems so as to make the functioning of hospitals and other healthcare systems more transparent. The public is becoming more aware of their healthcare requirements and options and is demanding more efficient and accessible healthcare systems, and the healthcare providers are becoming more aware of this need. Many healthcare IT firms are trying to fulfill this need, and are providing a variety of software services. Let’s try to understand the different types of healthcare software used by various healthcare providers.
EHR
Electronic health records or EHRs are used for storing patient information in a digital manner. It is used by hospitals and clinics to store the complete medical history of a patient. Government health regulators in many countries are moving forward with plans to make electronic health records mandatory.
These records provide a secure and easily accessible way of storing medical records compared to paper-based records. Electronic records do not have the risk of loss of medical history or being illegible or destroyed over a long period of time. It also prevents duplication of medical records, since there is only one file that is modified over time.
Electronic health record software is used in both clinics and hospitals and usually comes integrated with hospital management software and practice management software.
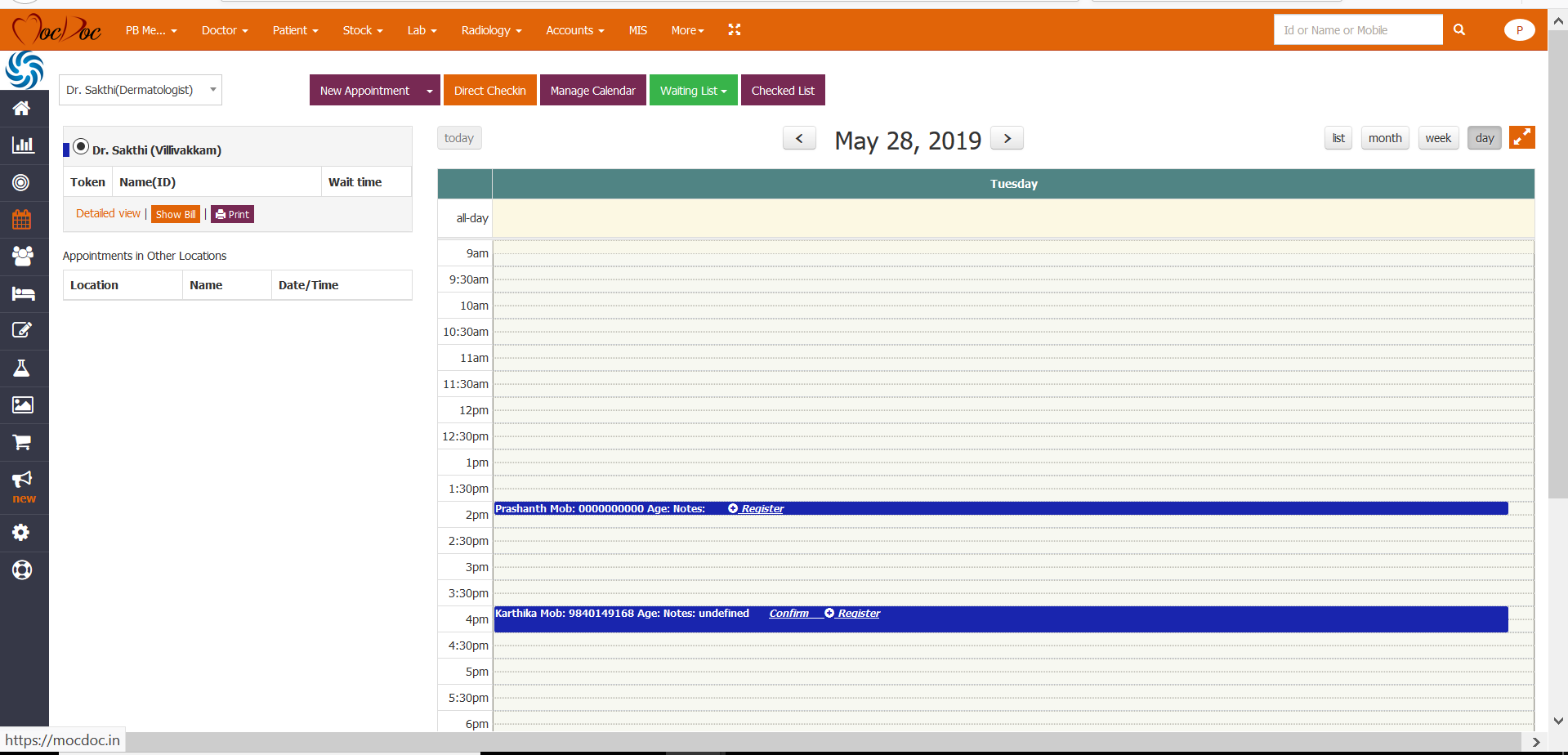
Practice management software ( PMS)
Practice management software or clinic management software is used for managing clinics. Depending on the requirement of the clinic, software with various combinations of features is available. Generally, they contain appointment management, billing, and electronic health records. Software with integrated lab and pharmacy management features is also available if there are labs or pharmacies associated with the clinic. Practice management software helps to streamline the workflow of a clinic, gets error-free documentation, manages appointments and billing, and makes the system more efficient.
Specialized systems are available for dental care, ophthalmology, and other specialty clinics, with customized prescription management and health records.
Queues in the clinic can also be managed by the system, either on the basis of tokens or on the basis of appointments
Hospital Management System ( HMS )
Hospital management system has almost all the features described above, and more. They are a fully integrated system capable of managing the entire hospital. They are capable of managing appointments and electronic health records for both inpatient and outpatient departments. They are used for managing doctors’ schedules, surgeries, other procedures, and all the aspects related to them. They are also capable of handling the labs and pharmacies attached to the hospitals. The HMS systems can also manage the rooms, marking rooms as occupied, unoccupied, undergoing maintenance, etc, making it easy to allocate rooms and beds for patients.
Hospital management systems are often linked to the websites of the hospitals and patients can use them to book their appointments, get access to their health records and treatment plans, and manage their prescriptions. These days they also come with apps for patients that aid the patients in these same tasks much more easily through their smartphones. Alerts are provided through SMS services for follow-up procedures, vaccinations, etc in some hospital management systems.
Due to the integrated nature of the HMS, all the procedures done in various departments of the hospitals, all the tests done, medicines administered, and prescribed are tracked, thus allowing easy comprehensive billing.
Laboratory information management systems ( LIMS )
Lab information management systems, as the name implies, are used to manage the functions of a lab. It will have provisions for sample collection, inventory management, accounting functions, and provisions for machine interfacing with the lab equipment.
A good lab information system will provide full automation and ensure error-free results, with alerts for abnormal results. With machine interfacing, data from the instruments in the lab are directly read by the software, and accurate records are made against the sample data. In the case of LIMS systems integrated with the hospital management system, provisions may be there to add the test results to the patient records. Stand-alone systems are also available for use by independent laboratories.
The Laboratory information management system helps lab technicians to achieve a smooth workflow and better quality control. From the point at which the sample is collected, till the results are delivered, samples are tracked using the software, which means that any technician in the lab can find out what to do with a sample at every step of the way, thus avoiding issues with sample management. The system also prevents errors, thus improving the credibility of the lab.
Billing software
Billing software has been used as part of hospitals and clinics ever since accounting went digital. Even before EHRs came, accounting software was being used in many hospitals.
Billing software helps to manage insurance claims and provides a smooth accounting of medical bills. The entire medical costs of all the patients can be easily accessed and organized in an efficient manner using billing software. Though they come along with hospital and practice management systems these days, they are still available as stand-alone systems.
Related Articles
Universal healthcare - let’s...
Universal health care is a hot topic for discussio..... Read more
How Technology Leverages Patie...
Imagine the following scenarios: An electroca..... Read more
Benefits of an Online Appointm...
Exploring The Benefits of Online Appointment Syste..... Read more
Introducing Ayushman Bharat Di...
Ayushman Bharat Digital Mission (ABDM) Th..... Read more